
End to end journey of the IDEAL CHD journey during interstage

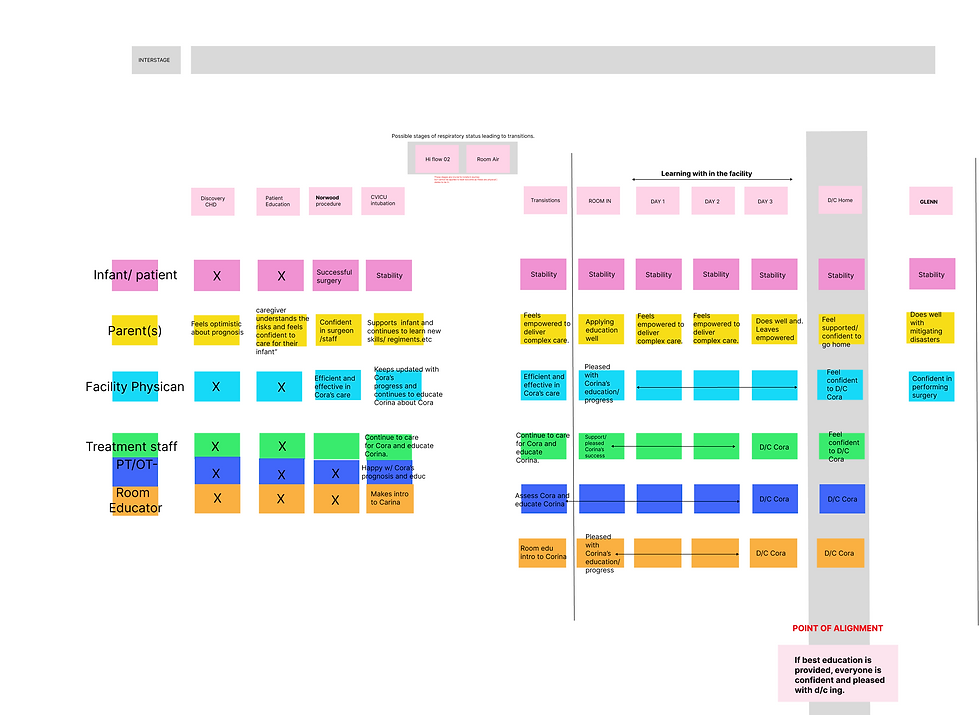
Service Outcomes per Stage
Project Background:
Congenital Heart Disease (CHD) affects approximately 1 in every 100 babies born in the United States each year. CHD is a lifelong journey that often begins with diagnosis in the prenatal period or at birth and lasts through adulthood. A quarter of these newborns will have severe or critical CHD that requires surgery or other procedures in the first year of life. Patients with CHD face years of complex and challenging medical care, which takes a toll on them and their families.
The Texas Center for Pediatric and Congenital Heart Disease is working to become a center of excellence for pediatric congenital heart disease in Central Texas. It has partnered with Dell Medical School's Value Institute for Health and Care and the Design Institute for Health better to characterize the journeys of patients and their families and create opportunities to redesign and improve patient care. Our project scope focuses on what is referred to as the interstage period occurring between a baby's first and second surgeries, the Norwood and the Glenn. At the same time, there are a few critical clinical milestones during the first hospital stay.
* It is essential to understand that interstage starts at 0-3 days old and continues over the next 4-10 months.
Project Goal:
Problem Statement:
During interstage there are different definitions of what success is.
For some success may be having no more seizures, or being able to be on room air, having a specific heart rate, being able to tolerate tube feeds etc.
Where do they align?
Improve the discharge process and define what success looks like to different families while trying to find points of alignment.
*Looking at the VBH care model,QOL is different for every patient and caregiver. Depending on the severity of the heart abnormalities, complications etc.
A Successful interstage journey is never the same.The overarching consensus is the education that is delivered
Summary:
This analysis was done working with speculations and in-depth research would need to be done to further solidify this hypothesis. That said, the common service outcome seems to be prioritizing efficiency of content and education.
This means making sure the proper material is developed and delivered for the caretakers to feel confident in their ability to make decisions in medical predicaments to intervene as best as they can. The physician sitting between the team and caretakers are obliged to attend to both stakeholders and facilitate success by properly delivering/training on the educational content.


Questions about the Service:
-
What type of learning program would satisfy the needs of the caregivers and business?
-
At what point do we teach that
caregivers sometimes encounter medical occurrences are out of our control? -
How do we ease the burden of “Guilt” when mortality occur?
-
How do we best prepare for typical vs non typical.
-
How do we involve language barriers?
-
How can we decide best KPIS to apply?
-
What does QOL look like for each user/ stakeholder?
Possible KPI's:
-
Bed turnover
-
Rate of recurrent admits
-
Rate of avoided issues due to early intervention.
-
Self scored assessments.

Mapping/Defining Ideal Outcomes
-
A Service outcome is the end result of a service NOT HOW you achieve it.
-
They should align to known strategic priorities. STRATEGY + SERVICE
-
WHAT are the factors that will lead to a successful project?
-
HOW: Do we align our design research activities such as journey mapping to our strategy?
-
WHY: Service outcomes are essentially core user needs that have been met – the result of what happens if this service or stage performs well.
-
For providers, outcomes are written as if this service or stage is run in the most efficient and effective way possible.